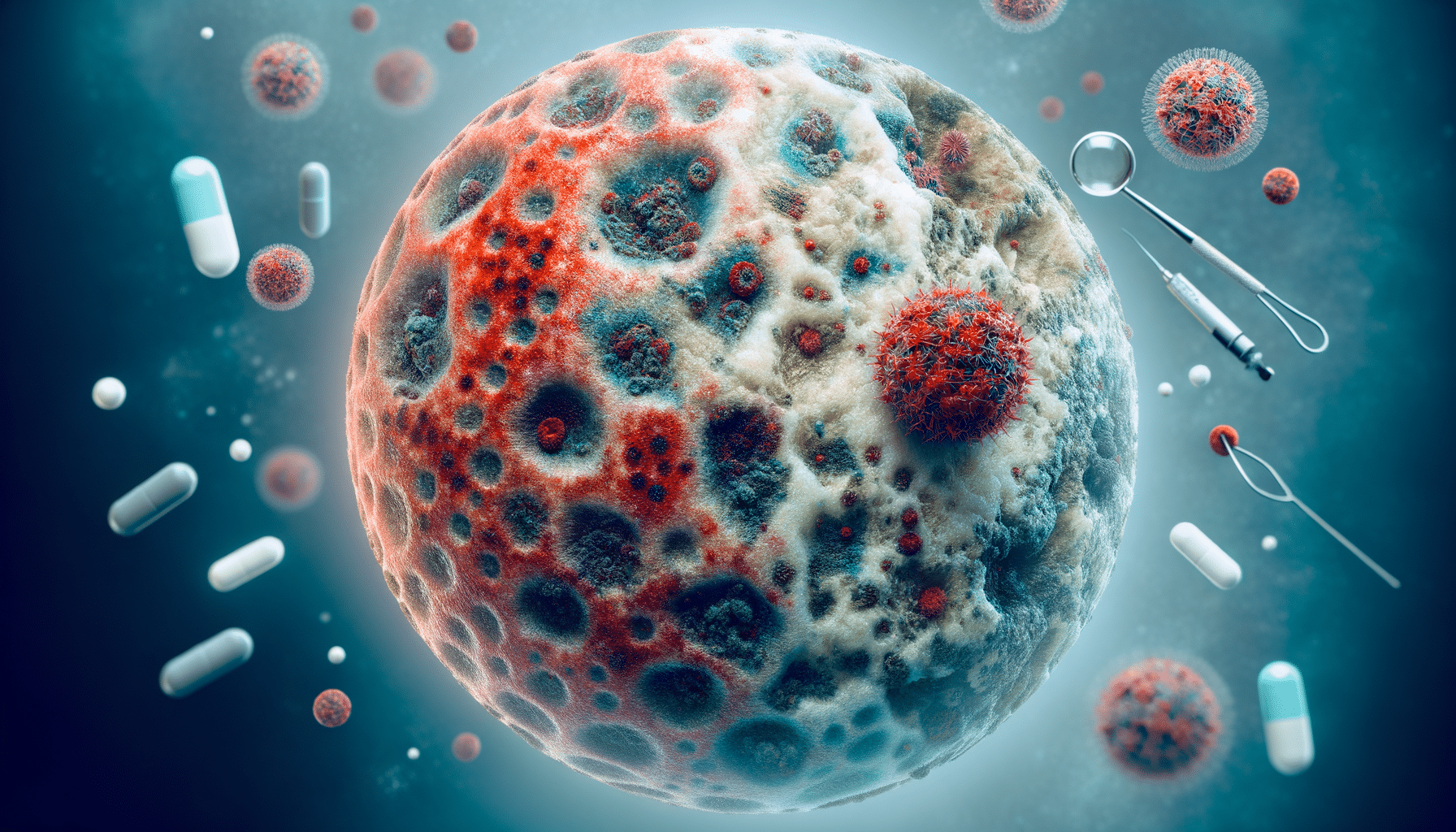
What a Mycosis Fungoides Rash Looks Like in the U S Early Signs and What to Know About Treatment
Understanding Mycosis Fungoides: An Overview
Mycosis fungoides is a rare form of non-Hodgkin’s lymphoma that primarily affects the skin. The condition is characterized by the presence of malignant T-cells, which are a type of white blood cell. These cells infiltrate the skin, leading to various dermatological symptoms. Understanding the early signs and symptoms is crucial for timely diagnosis and treatment.
In the United States, awareness about mycosis fungoides is growing, but many still find the condition perplexing due to its rarity and complex presentation. The disease progresses slowly, often over years, and can be mistaken for more common skin conditions like eczema or psoriasis. This misidentification can delay diagnosis, underscoring the importance of recognizing its unique characteristics.
Common symptoms include persistent skin rashes, patches, or plaques that may be itchy or scaly. These symptoms can evolve, making it essential for individuals to seek medical advice if they notice persistent or unusual skin changes. Early detection and treatment can significantly impact the progression and management of the disease.
Mycosis Fungoides Symptoms in the U.S.
The symptoms of mycosis fungoides can vary widely among individuals, but there are common signs to look out for. In its early stages, the condition often presents as a rash that can resemble eczema or dermatitis. This rash is typically red, scaly, and may be itchy. As the disease progresses, the rash can develop into thicker plaques or even tumors on the skin.
In the U.S., dermatologists and oncologists are increasingly aware of these symptoms due to improved education and resources. Patients may experience:
- Patches: Flat, scaly areas that can be mistaken for eczema or psoriasis.
- Plaques: Raised, thickened areas of skin that are often itchy and can vary in color.
- Tumors: Larger, nodular growths that can appear on the skin in advanced stages.
Recognizing these symptoms early can lead to a more accurate diagnosis and a better prognosis. Healthcare providers in the U.S. utilize a combination of skin biopsies and imaging studies to confirm the diagnosis and stage the disease, aiding in the development of an appropriate treatment plan.
Mycosis Fungoides Rash Identification
Identifying a mycosis fungoides rash can be challenging due to its similarity to other skin conditions. However, there are specific characteristics that can help differentiate it. The rash typically starts as small, flat patches that may be pink, red, or brown. Over time, these patches can become more pronounced and form plaques or nodular tumors.
In the U.S., dermatologists are trained to recognize these signs through careful examination and patient history. A biopsy is often necessary to confirm the presence of malignant T-cells in the skin. This diagnostic tool is crucial for distinguishing mycosis fungoides from benign skin conditions.
Patients are encouraged to monitor their skin for any changes and consult with a healthcare professional if they notice persistent or unusual rashes. Early identification of mycosis fungoides can lead to more effective management and treatment, potentially slowing the disease’s progression.
Treatment Options for Mycosis Fungoides in the U.S.
Treatment for mycosis fungoides varies depending on the stage and severity of the disease. In the United States, a range of options is available, from topical treatments to systemic therapies. The goal is to manage symptoms, slow disease progression, and improve the patient’s quality of life.
Common treatment options include:
- Topical Corticosteroids: Used to reduce inflammation and relieve itching.
- Phototherapy: Exposure to ultraviolet light can help control skin symptoms.
- Radiation Therapy: Targeted radiation can be effective for localized skin lesions.
- Systemic Therapies: Oral medications or injections that target the immune system or cancer cells.
Recent advancements in treatment have focused on targeted therapies that specifically address the malignant T-cells. Clinical trials in the U.S. continue to explore new drugs and treatment combinations, offering hope for improved outcomes.
Patients are encouraged to work closely with their healthcare team to develop a personalized treatment plan. Regular follow-ups and monitoring are essential to assess the effectiveness of the treatment and make necessary adjustments.
Conclusion: Navigating Mycosis Fungoides
Mycosis fungoides is a complex condition that requires careful attention and management. In the U.S., awareness and understanding of the disease are improving, leading to earlier diagnosis and more effective treatment options. Recognizing the symptoms and seeking medical advice promptly can significantly impact the course of the disease.
For those diagnosed with mycosis fungoides, a comprehensive approach that includes regular monitoring and a personalized treatment plan is crucial. As research continues to advance, there is hope for more targeted and effective therapies that can improve the quality of life for those affected by this rare form of non-Hodgkin’s lymphoma.
By staying informed and proactive, patients and healthcare providers can work together to navigate the challenges of mycosis fungoides, ensuring the best possible outcomes.